Proximal subungual onychomycosis is the least common onychomycosis in healthy persons though it occurs fairly often in immunocompromised individuals. One of the more unique features of proximal subungual onychomycosis is that the fungus invades the nail at the cuticle and becomes intimately associated with the nail bed. The disease moves along with the growing nail toward the tip.

Proximal subungual onychomycosis can cause a number of visible changes in the fingernail or toenail. In this disease, the nail plate becomes white and/or yellow near the cuticle. The distal portion of the nail (near the tip of the finger) is usually unaffected by the disease. This is especially true early in the course of proximal subungual onychomycosis. The fungus invades the nail rather deeply and can cause the nail bed (the soft fleshy area underneath the hard nail) to become bumpy and irregular. The nail near the cuticle is often destroyed as part of the disease process. As the nail grows it may have folds and pits. The combination of an irregular nail bed and misshapen nail plate may cause the nail to become loose.
Like distal subungual onychomycosis, most cases of proximal subungual onychomycosis are caused by a dermatophyte called Trichophyton rubrum. Another dermatophyte, Trichophyton mentagrophytes may be to blame in some case. Proximal subungual onychomycosis is sometimes caused by the invasion of molds.
Another curious feature of proximal subungual onychomycosis is that the skin surrounding the nail may become red, inflamed, and swollen. This is especially true if the disease is caused by molds. The nail and surrounding area may ooze pus in proximal subungual onychomycosis.

The inflammation and pus are what cause many physicians to incorrectly diagnose proximal subungual onychomycosis as a bacterial infection rather than a fungal infection. This can be a problem if antibiotics are prescribed since antibiotics do not kill fungi. An antifungal medication is required to kill dermatophytes, molds, and yeasts.
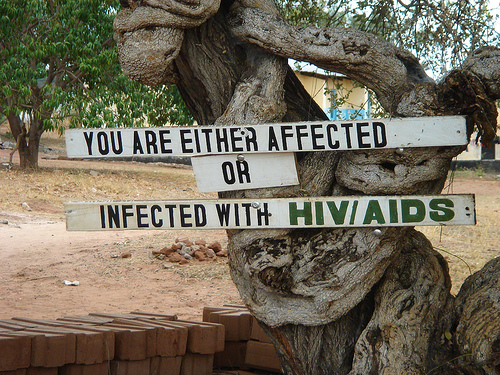
Proximal subungual onychomycosis is a fairly uncommon form of onychomycosis. It occurs most often in people with depressed or deficient immune systems. A person may have a depressed immune system due to certain blood cancers or because they are undergoing treatment for cancer like chemotherapy or radiation. Any immunosuppressive treatment can depress the immune system, by definition. Patients may be on an immunosuppressant if they are being treated for an autoimmune disease or have had an organ transplant and are on anti-rejection drugs.
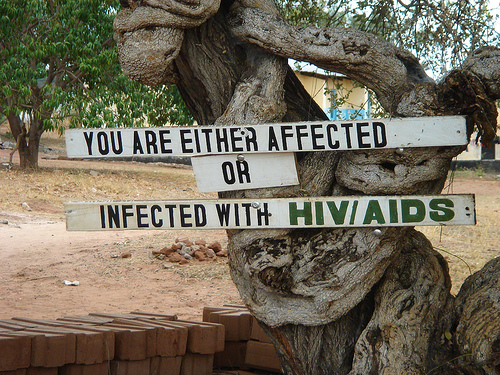
While proximal subungual onychomycosis can occur in any of these patient groups, it seems to occur particularly frequently in patients with human immunodeficiency virus or HIV. In fact, it occurs in this patient population so frequently that when proximal subungual onychomycosis occurs in a patient without an obvious reason for a suppressed immune system, the treating physician may suggest a test to check for HIV. If you are seeking treatment for a fungal infection of the fingernail or toenail that has started at the cuticle side of the nail, be prepared to be asked to have an HIV test. This test can only be performed with your consent. Also keep in mind that a diagnosis of proximal subungual onychomycosis does not necessarily mean that you have a diagnosis of HIV.
Unlike some other onychomycoses, proximal subungual onychomycosis simply must be treated with an oral antifungal medicine in order to eradicate the problem. There are a number of possible oral onychomycosis treatments, however they are only available by prescription in United States. Topical medications are completely ineffective in treating proximal subungual onychomycosis.
If the proximal subungual onychomycosis is known to be caused by Trichophyton rubrum or Trichophyton mentagrophytes, then a good treatment choice is terbinafine, also known as Lamisil. Terbinafine is given as a 250 mg pill once a day for six weeks if treating fingernails and twelve weeks if treating toenails. Lamisil has no effect on Candida infections and should not be used to treat cases of proximal subungual onychomycosis caused by this organism. Lamisil has the advantage of being less expensive than the other new generation of onychomycosis treatments.
Itraconazole (Sporanox) is a good option for proximal subungual onychomycosis when the cause of the disease is known to be fungal but may or may not be a dermatophyte. Sporanox has some activity against Candida, too. This treatment is usually more expensive than other onychomycosis treatments, including Lamisil.
Fluconazole (Diflucan) can be used to treat proximal subungual onychomycosis, but this is not a first line drug for this disease. This medication halts the growth and spread of the disease rather than killing the fungus outright. In medical terms, fluconazole is fungistatic (fungus stopping) rather than fungicidal (fugus killing).
This means that the drug helps the immune system get a handle on the fungus by slowing down its growth. Since many cases of proximal subungual onychomycosis occur in people that already have depressed immune systems, this approach may not be terribly effective. When used, fluconazole (Diflucan) treatment usually continues until symptoms resolve.
References
Hainer BL. Dermatophyte infections. Am Fam Physician 2003;67:101-108.
Jaffe R. Onychomycosis: recognition, diagnosis, and management. Arch Fam Med 1998;7:587-592.
Click Here For Highest Rated Nail Fungus Treatments
1. Funginix - www.Funginix.com
2. Zetaclear - www.Zetaclear.com
3. PurNail - www.Purnail.com

Fungal Nail Removal says:
It’s good to consider Laser Fungus Treatment. It cures fungal toenails in just 30 minutes. But it costs a lot… at least here in Toronto.
elen says:
i have this fungus from three years and i still have it so i tried all
this treatment Lamisil and sporanox but nothing really worked so i am
thinking of removing all the infected nail but i heared that the fungus
will return as if i did nothing so please can help me i have this
fungus in five of my fingernail and three in my toenail. thanks
Tim says:
I have had this fungus for two years. But it’s starting to clear up. My treatment is to sand the nail gently and apply terbinafine (Lamisil) cream morning and night, In between – and after my morning swim, I soak the nail in tea tree oil. This combination seems to work but you have to be persistent and not let up for a minute. Wear Birkenstocks (or similar) without socks whenever you can.
ronnie guy says:
i got terbenafine pills and it almost killed me the company who
creats this should be closed and be in jail for murder attempt
the doctor who gave me did not test my liver or anything at all
this horrible thing happened in sweden.never trust a swedish
doctor especially if you are an immigrant.do not take any pills if
you wish to live.watch-out in europe doctors kill many people
and nobody seems to care.if you are dark be very carfull
the nazzies are everywhere and they can look very cute.
my advice go to chinese herb doctor and only use natural
medicine avoid all these develish medicine industry and never
trust them dont forget mother nature…….
Nasi says:
My husband has had nail fungus for many years and he has been using lamisil, but it never has cured it on a permanent basis. On the other hand, it has side effects. Please try natural way or try to make your system stronger.
LLexy says:
I have this proximal-subungual-onychomycosis on one of my toenails for about a year now (untreated… as I didnt know what it was and was trying to ignore it). I have had two HIV tests which were negative, over the past 6 months. From what I have read about this proximal-subungual-onychomycosis….. the experts appear to be saying that everyone who has a proximal-subungual-onychomycosis fungis is HIV positive. Is this true? Do I need to rush out and have ANOTHER HIV test?
Marilyn says:
Zeta clear does not work! Don’t waste your money on it.